Shaping the future of healthcare: Data, AI and Us
8 May 2024
Mike Beck, our Head of Electronics spent some time in Boston at the Device Talks Conference last week. Here are…

Human Factors Considerations For Your Emergency Use Drug Delivery Device
6 December 2023
Emergency use devices have been a long-standing part of the drug-device combination product market, with early autoinjectors being developed for…

Designing for Good: Harnessing the Power of UX for Social Impact
5 December 2023
User experience (UX) design has become a critical element in shaping how people interact with devices. Beyond creating aesthetically pleasing…

Tips and tricks for user-centric design
27 September 2023
Leanne Yip, Head of Design and Usability outlines some tips and tricks for designing patient-centric medical devices. As humans, we…
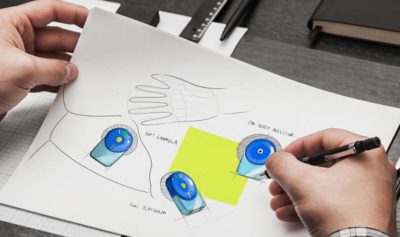
5 key reasons to use industrial design when developing a product
19 September 2023
Industrial design drives innovation and builds business success. It’s not just about making things look good, but also about making…

Product design, user experience and gender equality – can it work?
8 March 2023
The theme for International Women’s Day this year focusses on gender equality. We want to take a look at how…

UX design can make or break your product
7 February 2023
UX design to influence a change in behaviour from the user and how that can be used to improve adherence…

The future of diabetes care with a user-centered approach
15 August 2022
MedTech Navigator’s “The Future of Diabetes Care” seminar highlighted that whilst developments in the treatment of diabetes have been extraordinary…

The wrong user interface can be unbearable to use. How can you avoid this?
21 April 2022
User experience (UX) explores how a customer interacts with a system, and how they feel when using it. The UX…